It’s been one of those weeks where a number of seemingly unconnected events have been signs pointing me in a single direction.
I had a conversation with a friend on Monday (one which I will inaccurately paraphrase here) about the concept of a fear prison. The concept as I understood it describes the moments when something becomes legal, permissible, even encouraged, but we are unable to embrace, accept or even explore it because we remain trapped in the FEAR of horrible consequences. The fear remains, despite our logic brains reminding us that the actual danger has passed. We can remain trapped, capturing ourselves into custom built, highly individualized fear prisons. No amount of intellectual reasoning or reassurance from friends and family can truly convince us that the danger has passed, that we are safe and that the “risk” we perceive as insurmountable is, in fact, no longer a risk at all. The fear prison is both irrational (because no actual danger exists) and extremely rational (because it exists based on threats which were at one time real). The fact that it simultaneously FEELS real and is in fact not true, makes it a particularly challenging concept to work with.
As a survivor of abuse, sexual assault, family violence, relationship abuse and systemic discrimination and institutional violence caused by the very systems that were presented as existing to protect survivors, I have built a complex and sturdy fear prison.
This fear prison is the driving force behind, and explanation for, so many of my decisions and so many of the symptoms of PTSD which weigh down my mind, body and spirit.
Just under two months ago, my ex-husband signed court documents which were stamped and sealed by a judge, giving me sole legal custody of my two children. In reality, this piece of paper opened the doors of a real prison. It represented an actual, tangible increase in safety, decision making power and freedom of choice. People in my life, knowing how long and hard I’ve fought for this piece of paper, celebrated for me. They were happy and congratulated me for “winning” after a long fight.
I think many people are confused and somewhat disappointed by my inability to celebrate. I don’t feel relieved. I don’t feel safe. I don’t feel like I have won ANYTHING. I don’t find it easier to make decisions. I don’t feel free.
I’m still caught in my fear prison.
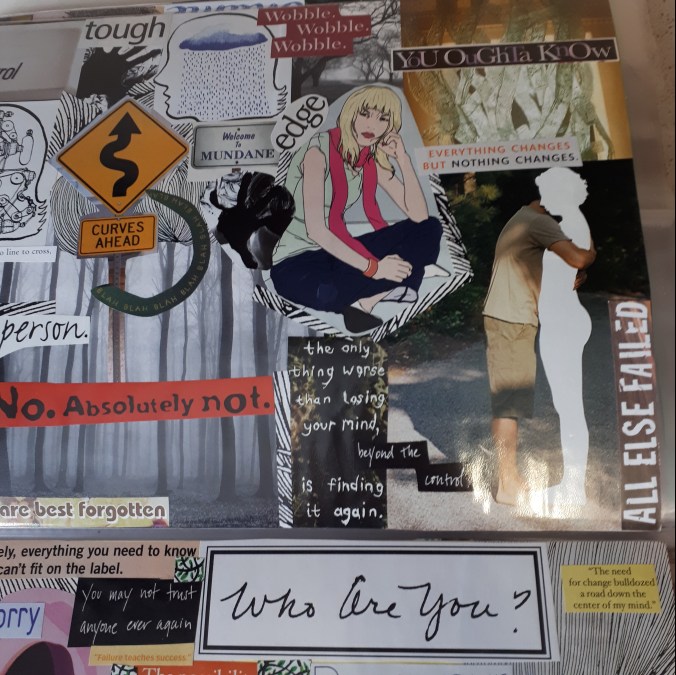
The walls of the prison are built by a trifecta of related fears.
First, the fear that I can’t trust him and can’t trust the unpredictable nature of violence. This is the fear that he might come back, that he might try to hurt me or hurt my children when I least expect it. The fear that if I let my guard down and allow a feeling of safety to exist, that I will be most at risk. This is entwined with a fear that if I allow myself to relax and feel happiness or relief that it will be taken away from me: swiftly, without warning and in a terrifying manner. This is the fear that every decision I make, every plan I make, every step forward I take, everything I build can be taken away. That it will be MY fault it is taken away because I foolishly let myself believe I was safe.
Second, the fear that I can’t trust anyone. The fear that if I’m honest with doctors about how I feel then they will judge me and find me wanting. The fear that people don’t believe me about the events of my life and my experiences. The fear that people find me annoying, whiny, controlling, and generally too needy. The fear that if I open up, I will risk being hurt again. The fear that honesty will result in terrible consequences and that I should be careful about sharing TOO much or needing TOO much because it might result in me losing my children. This fear at a deeper levels is that other people believe that I am crazy, insane, mentally ill, hysterical or mad.
Third, the fear that rules them all, is the fear that I cannot trust myself. The fear that I am crazy, broken, damaged and maybe delusional. The fear that I can’t trust my own memories of the past. The fear that I exaggerated or invented the abuse. The fear that I’ve accused innocent people of crimes they didn’t actually commit. The fear that I’m making too much out of too little and that a “normal” person wouldn’t react this way, have these thoughts or these experiences. The fear that all of the challenges, abuse and violence in my life have been either my own fault or creations of my own mentally ill mind. This fear keeps me frozen, analyzing and picking apart all my flaws and potential flaws. This fear fills me with shame and makes me feel worthless. Or maybe I feel ashamed and worthless because of this fear.
Believing that others think you are crazy, that you can’t trust others and that you can’t trust yourself because you might actually BE crazy builds up an extremely secure fear prison. A fear prison so strong, that no amount of reality, court orders, locks on doors, or distance can break down.
This fear prison can only be dismantled through my own healing process. By gradually challenging my fearful thoughts and looking for evidence that my fears are no longer true or real. It may be that some of the fears were NEVER true or real, but were creations of my abusers, projected on me and designed, plotted and crafted to drive me insane.
The path to “winning” is not in the court orders or external victories. The winning is my stubborn refusal to give up. The winning is staying alive despite the intense desire to die. The winning is getting up each morning and living my life, in spite of the fears. The winning is parenting and protecting my children each day. The winning is behaving as if I’m valid and sane, even when I believe I am worthless and crazy. The winning is reminding myself that I am a good person and that only a very BAD person would abuse someone and gaslight them hoping they would kill themselves so they could be proven “right.”
In his mind, the only way my ex-husband can be proven right, be proven not to be an abuser, be proven to be righteous and a good person, is for me to kill myself. If I kill myself it proves to him that I am, and have always been, CRAZY. If I die, his narrative becomes the truth and my accusations become just the ramblings of a mentally unstable person, not to be trusted. I will live forever just to prove him wrong!
There are reasons I have my particular type of fear prison. I fear that I am crazy because I was led to believe this. I was led to believe I was crazy by abusers who gaslighted me. I was led to believe I was crazy by doctors who labelled me as borderline. I was led to believe I was crazy by the police officer who never properly investigated my report of sexual assault. I was led to believe I was crazy by the doctors and school principals who lied, under OATH, during my family law trial. I was led to believe I was crazy by child protection workers who told me that I was projecting my anxiety onto my children and that I needed to be more neutral in my reactions towards my ex-husband’s transphobic violence. I was led to believe I was crazy by family law judges, who denied that I had been abused (or denied that it was relevant to the custody arrangements). The entire system, from the moment I was first assaulted (and even before) has been a set up to create in me the belief that I can’t trust myself, my memories, my body or my mind.
Breaking down my fear prison means trusting myself. Breaking down the fear prison means living as if I am sane. Breaking down the fear prison means that my memories are true and that the injustices I’ve survived actually happened. Breaking down my fear prison means accepting that so much of the violence was completely and utterly out of my control. That is TERRIFYING. Believing that I was helpless to stop it and that it wasn’t my fault is terrifying. Believing that I did everything I could and that I did my absolute best at every step and that I still was powerless to stop the abuse is terrifying.
But not as terrifying as the fear prison of believing that I am crazy.
I’m not crazy.
 It was created by an artist Hannah Daisy @makedaisychains (photo credit to her.
It was created by an artist Hannah Daisy @makedaisychains (photo credit to her.