I’d like to share some ideas for readers who have struggled with, or currently struggle with, self harming behaviour of any kind. Self harm can include physical injuring, substance abuse, eating disorder habits, workaholism, over exercise etc.
Personally, I find harm reduction models to be the most effective in reducing self harming behaviour. Because self harming is a coping method, and has served a purpose, it is often difficult to abstain from doing it. I also believe that the majority of habitual self harming behaviour is shame and avoidance based in at least some ways. I have found it easier to live with the idea that I will sometimes engage in behaviours that are not 100% beneficial to my health. By acknowledging this openly, I reduce the level of shame I feel when I do make a mistake, slip or relapse. Relapse is a part of recovery in a harm reduction model. I don’t need to feel ashamed if I go back to my old way of coping in a crisis. Those ways worked for me for a long time and they are habitual and comfortable to slip into.
If I have a slip, I don’t make a big deal about it. I just move forward and try to make a different more self caring choice in the future. Removing the intense lens of self judgment from the situation has been helpful for me.
When suggesting alternatives to self harming behaviours, I acknowledge openly that not all options are available to all people. This is not a list that says “you should do this” but just some options that have worked for me personally. Using the word “should” can increase feelings of guilt and shame if you do engage in self harm. I highly encourage you to use this as a model, and make your own list that feels right for you. Give yourself permission to explore different coping options, keep the ones that work and leave the ones that do not. Personalizing your recovery plan is another factor that will lead to greater success within harm reduction.
- Give yourself permission to struggle. It’s okay that you feel bad right now. Your feelings will have a beginning, a middle and an end and you can survive them. Sitting with your feelings is an option, even if it is very uncomfortable
- Get safe. Often urges to self harm are a red flag for me that I’m not feeling safe or I’m feeling overwhelmed. Reduce any stress you have control over. Relocate to an environment that feels secure.
- Spend time in nature. The trees are not oppressive, nature is forgiving. Nature can just mean getting outside, walking around the block, sitting in a park and breathing deeply. Noticing the colours in the leaves outside.
- Wrap yourself up in warm blankets, quilts, cozy sweaters etc. For me feeling safe often involves feeling warm and wrapped up tight. Sometimes even the weight of the blankets is calming to me
- Prepare a hot or cold beverage. The warmth or chill of the cup in your hands can help to ground you. Focus on the temperature of the glass, and the feeling of the cold or warm liquid in your mouth. Taste the flavours in your drink and take time to breathe.
- Draw, scribble, write, paint -express your feelings. Artistic self expression has helped me avoid self harm. You don’t need to be an artist to do this, you don’t need expensive art supplies. Sometimes just a piece of paper and pen is enough. Feel free to destroy your creation after.
- Reach out. Call a friend, a family member, a support or crisis line. If you don’t feel comfortable calling anyone, try going to a public place like a library or coffee shop and just break the isolation by sitting there with people around you. Talking to a safe person is often a good way to work through urges to self harm. You have the choice to tell the person you are struggling or not.
- Distract yourself with an enjoyable TV show, youtube video, magazine, book or music. Lose yourself in another world for a short time. Choose something that will cheer you, not something triggering.
- Exercise. Use your large muscle groups. Walk, do jumping jacks, stretch, yoga, lifting cans in your kitchen, anything you feel able to do and have access to. Moving your body can help you process intense feelings like anger.
- Connect with spirituality, meditate, religion etc. Connect with a higher power. For me this means visiting nature and getting in touch with how small I am compared with the power of the natural world
- Spend time with someone very young or very old, or a pet. Volunteer, connect with a family member, visit a neighbour with a new baby, offer to pick up groceries for a senior living in your area. Walk your neighbour’s dog, take care of your own pets. Helping others, even in small ways, can be an option and alternative to self destructive coping. For me, being able to help another person reduces my sense of shame and hopelessness and increases my connections.
- Hug a stuffed animal. Sometimes I need comfort and stuffed animals are a good option for me and help me feel safe.
- Spend time around water. Take a bath or shower. Walk by the river, ocean or lake. Go swimming. Run warm or cold water over your hands and wrists. Flowing water can be very calming.
- Use positive affirmations, ideally ones you have prepared yourself. Sometimes self harming is driven by negative self talk and negative shame based messages you are giving yourself. You can find ideas for affirmations on the internet and rework them to suit your purpose. If an affirmation seems unrealistic try adding “I’m learning to…” at the beginning. For example, “I’m learning to love myself.“
- Remind yourself that you are doing the best you can. That you are surviving and sometimes that is enough. Some days all we can do is survive and that’s okay.
These are just a few ideas I’ve worked with over the years. I hope you find them helpful. Please feel free to comment with your coping ideas!



![20160823_195012[1]](https://hopeforsanityblog.com/wp-content/uploads/2016/08/20160823_1950121.jpg?w=676)


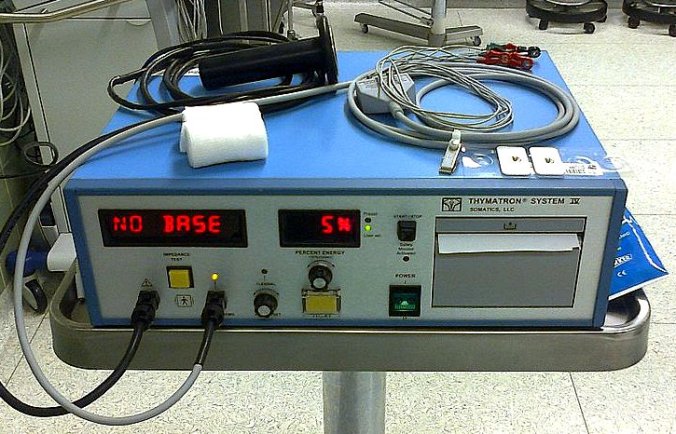
![20160727_214408[1]](https://hopeforsanityblog.com/wp-content/uploads/2016/07/20160727_2144081.jpg?w=676) One of the bright sides of spending so much time in hospitals during my teens and early twenties is the people I met there. Some of them became lasting friends and the bonds between us defied understanding by outsiders.
One of the bright sides of spending so much time in hospitals during my teens and early twenties is the people I met there. Some of them became lasting friends and the bonds between us defied understanding by outsiders.![20160724_170912[1]](https://hopeforsanityblog.com/wp-content/uploads/2016/07/20160724_1709121.jpg?w=676)